We all heard the term metabolism, which is the balance of all the chemical reactions that are happening in the body. There are biochemical reactions in every cell that are trying to build up molecules, which are called anabolic reactions or anabolism, and there are chemical biochemical processes that are degrading molecules breaking them down which is catabolism. Metabolism is the sum or the balance of all those anabolic and catabolic reactions.
Insulin is one of the body’s primary anabolic hormones. Its core role is to signal the “fed state” and shift metabolism away from catabolism and toward anabolism.
Insulin is a peptide hormone made by the beta cells of the pancreas and as it circulates in the blood it will come and bind on receptors of every single cell of the body from brain cells to bone cells, from lung cells to liver cells, and every cell in between them all have insulin receptors. The receptor is essentially a doorway that is built for insulin to come and knock on it.
What is insulin resistance?
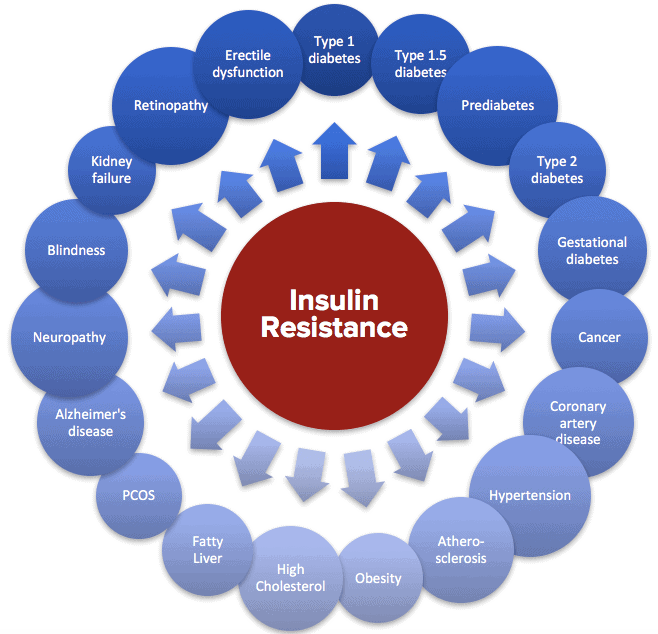
Insulin resistance is very important because of its relevance - every single chronic disease is in some way influenced by insulin resistance where insulin resistance is either directly causing the disorder, or it is facilitating the disorder.
Insulin resistance is a disorder with really two parts.
- Cellular level - Insulin resistance occurs when some of these cells are not responding to insulin anymore as well as they used to, they've become resistant to that knock. Let's say the insulin used to knock on the liver cell receptor, and the “door” would open right up, and liver would respond appropriately it would do what insulin asked it to do. However, over time due to insults the knock falls on “deaf ears” and the liver cell doesn't open the door all the time or maybe it'll open at a crack, ultimately it doesn't actually do everything insulin wants it to do. This is the state of insulin resistance. However, not every cell becomes insulin resistant. This is not a universal phenomenon within the body. Some cells of the body fail to respond to insulin as effectively as they used to, becoming less sensitive to insulin.
- Whole body – Hyperinsulinemia. The second aspect of insulin resistance that is often overlooked is that in every instance of insulin resistance, insulin levels will also be elevated in the blood. Therefore, the terms insulin resistance and hyperinsulinemia (elevated blood insulin) are inseparable. They will always occur together just like two sides of a coin. Hyperinsulinemia is relevant because there are some cells that are still insulin sensitive as ever, which are now overstimulated. There is a heightened response to the insulin because there's too much insulin relative to normal healthy insulin sensitive levels
Consequently, in insulin resistance some cells aren't responding to insulin anymore and at the whole-body level blood insulin levels are higher than they should be.
What is Metabolic Syndrome?
Metabolic syndrome affects roughly half of all adults across the entire planet, making it the single most prevalent disease or health disorder in the world. Metabolic syndrome is a cluster of complications, in particular five disorders that were noticed over the years to always clump together:
- High blood glucose – glucose is the building block of carbohydrates. When glucose is high our body's having a hard time clearing the glucose as you eat it, which will linger in the blood. This state is called hyperglycemia, and it is pathogenic since it will hurt your body, i.e., blood vessels, neurons, etc.
- High waist circumference - evokes this idea of storing fat more centrally particularly in the visceral space. More visceral fat contributes to higher inflammation and more general poor metabolic health.
- High triglycerides - is a feature of the metabolic syndrome that is a very good predictor of heart disease risk. As the liver starts to suffer, it begins to overproduce triglycerides and reduces the level of HDL.
- Low HDL – This is considered to be the good or the beneficial version of carrier of cholesterol. As the liver starts to suffer, it increases the clearance of HDL and overproduces triglycerides.
- High blood pressure - is directly related to and a consequence of metabolic health
Those are the five complications that make up the metabolic syndrome, and they all share one common point which is insulin resistance. In fact, the initial name of this cluster of complications was insulin resistance syndrome, which I prefer because it clarifies the cause and mechanism, as well as what needs to change to restore metabolic health. Metabolic syndrome is very vague. When you hear the term metabolic syndrome you do not know what you could do about it.
What Constitutes Metabolic Health?
Metabolic health can be explained through the lens of the metabolic syndrome or through the lens of metabolic flexibility, both mechanisms helping us understand the scope of the problem.
Metabolic flexibility, which is the ability of the body to shift readily between the two primary fuel sources: fats and glucose. There are times when the body is primarily burning fat and there are other times when the body is primarily burning sugar or glucose. For example, if you were to eat a mixed macronutrient meal made of carbs, fats and proteins, because of the carbs especially, you should expect that the body would shift primarily to sugar burning. That would be even more the case if you just ate pure carbs, then the body would heavily shift to sugar burning after that meal, aka post prandial state.
If you give your body approximately twelve hours or when you wake up the next day, by then the body should be in fasted state and it should have shifted over into fat burning mode. This shift would be a healthy response, known as metabolic flexibility.
However, some patients have developed metabolic inflexibility. Even when they have not been eating and are in a fasted state, they are not transitioning out of sugar burning and cannot enter into the fat burning state. They remain stuck primarily in sugar burning state.
Metabolic inflexibility is caused by the chronic elevated insulin, since insulin determines which fuel is going to be used. If insulin is elevated the body is obligatory in sugar burning mode. When insulin is low then the body goes into fat burning mode. Insulin is the single most important variable that dictates which fuel is going to be used.
The longer insulin is reduced, and the body is in fat burning mode, the more the body begins to burn more fat than it needs to meet its metabolic needs. Specifically, if insulin has been reduced for a substantial period, the liver burns so burns more fat than it needs to meet its own energetic needs and that excess becomes ketones. This process is called ketogenesis.
Ketones can be considered a surrogate marker of metabolic flexibility or metabolic health. Let’s say you have fasted for 16 hours, and you measure your blood sugar and ketone, and you find that your blood ketone levels are still low or undetectable that suggests that you have high insulin levels preventing fat burning and production of ketones. This is metabolic inflexibility.
In contrast if you've fasted for about 16 or more hours and you do see that you have entered into a higher level of ketones, that in this fasted state you had shifted to fat burning, then you can be pretty confident that you have good metabolic flexibility. This gives you confidence that you have good insulin sensitivity.
How Common Is Insulin Resistance and Why Has It Become the Single Most Common Health Problem Worldwide?
Our general biomedical view and the clinical approach to insulin resistance have inadvertently made the problem worse. In this case, most medically trained individuals selectively looked at certain aspects of the science surrounding insulin resistance and unwittingly accelerated the problem. We are looking at insulin resistance as a glucose problem ignoring that insulin levels are higher by necessity because insulin isn't working very well. And the elevated insulin is both cause and consequence. This is a cardinal feature of insulin resistance. The body must increase insulin to keep glucose levels in check.
These individuals may be manifesting year over year various signs and symptoms of insulin resistance i.e., higher blood pressure, dyslipidemia, elevated waist circumference. If the doctors only measure the glucose that comes back normal every time, the doctors may conclude that everything's fine. However, if they were to expand their view of the problem to include insulin as a marker, they would find that insulin levels can be elevated up to 20 years before glucose levels ever start to change.
The elevated insulin level is the early warning that something is wrong. Thus, our glucose centric paradigm or glucose obsessed view of metabolic health misses the problem. If we had rather an insulin centric perspective, we would have detected the problem at its earliest stages.
Our failure to focus on insulin resulted in our inability to diagnose the problem as early as we could, which has inadvertently resulted in therapeutic interventions that make the problem worse. For example, if a person who now is struggling with their elevated glucose levels, has 4 to 5 times higher insulin levels than it used to be, and still is unable to keep the glucose within normal range, may be given injectable insulin or oral medication that force the pancreas to make more insulin under this glucose centric paradigm.
This approach will push the insulin up even higher, which will lower the glucose, so the clinician feels better about that. But the patient will not feel better because these interventions make the insulin resistance worse and all of the chronic diseases also get worse including weight gain, heart disease, Alzheimer's disease, cancers, and ultimately death because insulin resistance is the key problem, it's not the elevated glucose. This is one reason why insulin resistance has become so common because we look at it incorrectly.
Lastly, it's simply just our lifestyle that led to the creation of this perfect metabolic storm. We have a host of variables specifically working against us, such as our dietary habits, what we eat and how frequently we eat, our poor sleep habits, our chronic stress, toxic exposures, etc. that trigger and perpetuate the insulin resistance and metabolic syndrome.
Checking for Insulin Resistance and Metabolic Syndrome
I encourage you to measure your glucose and ketone levels upon awakening to find out if you have insulin resistance. If your 12 hrs. fasting glucose is between 75-85 mg/dL and your ketones are 0.5 mmol/L or higher, you do not have insulin resistance. You can get the most accurate readings using a Keto Mojo meter that requires a finger prick. However, you can measure your ketone levels in your breath or your urine, but those results are affected by several factors.
BASIC STARTER KIT - GK+ Blood Glucose & Ketone Meter – Keto-Mojo USA
If your 12 hrs. fasting glucose is in the 90s or higher and ketones are lower than 0.5 or undetectable, you are on your way to or have developed insulin resistance. Testing again after 16 hrs. of fasting will help you see how advanced your metabolic syndrome is.
If you have been told that you have high blood pressure and/or your skin around neck or on other skin folds has changed texture or became darker (aka acanthosis nigricans) or have skin tags (mushroom like stocks of skin), these are proof positive of insulin resistance.
Remember, insulin resistance can be reversed, and your metabolic flexibility can be restored. GlucoNutrients was specifically designed to improve insulin sensitivity and reduce hyperglycemia.
If you or someone you love suffers from insulin resistance or metabolic syndrome, act now. Make an appointment for Integrative Functional Medicine evaluation for a renewed, healthier, and happier life.
Resources
1) Reaven, G. M. (1988). Role of insulin resistance in human disease Pacific Heart, Lung & Blood Institute Workshop https://en.wikipedia.org/wiki/Gerald_ReavenWikipedia
2) Petersen MC & Shulman GI (2017). Mechanisms of Insulin Action and Insulin Resistance Physiology Reviews https://journals.physiology.org/doi/full/10.1152/physrev.00063.2017
3) Shulman GI (2000). Cellular Mechanisms of Insulin Resistance Proceedings of the National Academy of Sciences https://www.pnas.org/content/97/12/6656
4) Expert Panel on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults (1998). Clinical Guidelines NIH report via NCBI https://www.ncbi.nlm.nih.gov/books/NBK2003/